Medicine blended assesment( May)
I have been given the following cases to solve in an attempt to understand the topic of 'patient clinical data analysis' to develop my competency in reading and comprehending the clinical data including history,clinical findings, investigations, and diagnosis and come up with a treatment plan.
This is the link of questions asked regarding the cases:
Below are my answers to the assignment based on my comprehension of the cases.
1- PULMONOLOGY:
Patient details:
Questions 1:
What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
The following is the event timeline of symptom occurrences in the patient:
1st episode of SOB 20 years ago was of Grade 2. Lasted one week. Relieved on medication
Next 8 years, similar events every January which lasted 1 week, grade 2 severity. Relieved on medication
Was diagnosed with Diabetes 18 years ago
2nd severe episode of SOB 12 years ago and was of grade 2 type. Lasted 20 days. Relieved on hospitalization and treatment
Next 12 years, each SOB incident started every January and lasted 30 days
Latest episode started one month ago in April, is persistent since 30 days with grade 3 dyspnea.
20 days ago, She was diagnosed with Hypertension
15 days ago she started developing pedal edema and facial puffiness
Since 2 days ago, severity of breathlessness went up to grade 4 dyspnea (SOB at rest) not relieved on Nebulization along with decreased urine output and drowsiness.
Anatomical localization:
Right paracardiac localization of COPD
The possible etiological factors could be the following:
Exposure to allergens which could make it a possible occupational hazard
Infections by Moraxella, H. influenzae or Pneumococcus
Dust or pesticides exposure
Question 2 :
What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:
The pharmacological and non pharmacological intervention provided include the following:
Furosemide :
MOA: Blocking Na-K-Cl co transporter in loop of Henle > loss of K, Na and Cl in urine
Indication: 2D Echo was suggestive of potential development of Right Heart failure
Efficacy: Furosemide is the Ideal for the loop diuretic therapy in Heart failure
Budisonide
MOA: Inhibit inflammatory cytokine production
Indication: The dyspnea that was suggestive of COPD
Efficacy : Budesonide/formoterol reduced the mean number of severe exacerbations per patient per year by 24% versus placebo and 23% versus formoterol.
Ipratropium Bromide
MOA: bronchodilation and inhibition of mucous secretions
Indication: The dyspnea that was suggestive of COPD
Efficacy : Ipratropium controls the acute Exacerbation of COPD
Amoxicillin/clavulanic acid
MOA: bacteriostatic + Beta-Lactamase inhibition
Indication: Possibility of an infectious etiology for acute exacerbation of COPD
Human Actrapid insulin
MOA: Inhibition of glucose output by liver with simultaneous glucose uptake via the muscles
Indication: known case of Diabetes Mellitus
Head end elevation
Indication: Presence of Dyspnea
Efficacy: The high dynamic compliance value was observed with head end elevation .
Question 3:
What could be the causes for her current acute exacerbation?
Answer:
The possible causes of her acute exacerbation can be due to the following:
Exposure to allergens which could make it a possible occupational hazard
Infections by Moraxella, H. influenzae or Pneumococcus (Bacterial), Influenza, Rhinovirus, Coronavirus (Viral)
Dust or pesticides exposure
Question 4:
Could the ATT have affected her symptoms? If so how?
Answer:
The ATT could have been the reason for generalized weakness
Question 5:
What could be the causes for her electrolyte imbalance?
Answer:
The cause of Hyponatraemia and Hypochloremia can be due vigorous high ceiling diuretic therapy in order to control right heart failure.
2-NEUROLOGY:
A)
patient details:
QUESTIONS:
1)
Answer:
a) Symptomatology in the patient in terms of an event timeline :
1 year back :
History of 2-3 episodes of seizures 1 year back
4 months back :
Cessation of alcohol for 24 hrs
1 episode of seizure (most probably a GTCS)
Associated with restlessness, sweating, tremors
10 days back :
Generalized body pains
9 days back :
Stopped consuming alcohol since this day due to generalised body pains on the previous day
-Started talking to himself and laughing to himself (sudden onset)
-Conscious , but oriented to time, place and person only from time to time
-Unable to lift himself from bed and move around
-Decrease in food intake
-Short term memory loss and unable to identify family members from time to time
Taken to a local RMP, given I.V fluids and reffered to a higher care facility
Admitted to tertiary care hospital on 15th may
b) Anatomical localisation of the problem :
- Acute symmetrical lesions in thalamus , mamillary bodies , tectal plates , periaqueductal area , floor of 4rth ventricle (includes occulomotor and vestibular nuclei and cerebellar vermis)
- lesions in the form of vascular congestion, microglial perforation and petechial hemorrhages.
c) Primary etiology for the patient's condition:
- Primary etiology for the patient's conditions is chronic alcoholism and dependance
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:
Inj. 1amp Thiamine in 100ml NS,TID
Thiamine deficiency leads to wernicke's encephalopathy and the administration of thiamine has been recommended as one of the first treatment modalities in wernicke's.
Indication of thiamine:
Thiamine has been recommended to be used to wernicke's to combat the deficiency of thiamine in the patient presenting with wernicke's
Inj. Lorazepam
Seizure prophylaxis with lorazepam injection is a commonly followed intervention in alcohol withdrawal seizures. Lorazepam binds to benzodiazepine receptors in post synaptic GABA-A chloride channels and increases the condction of chloride ions thereby enhancing the inhibitory actions of GABA.
Indications of lorazepam: Lorazepam is used in alcohol withdrawal in cases of
• patients with severe liver dysfunction
• elderly patients
T.Pregabalin
Pregabalin is a novel GABA-analogue approved for the treatment of alcohol withdrawal, partial onset seizures, neuropathic pain, and general anxiety disorder
Indications:
•Associated psychiatric symptoms in patients with alcohol withdrawal symptoms
•Seizure prone patients of alcohol withdrawal
•Anxiety, hostility and psychoticism in patients of alcohol withdrawal
Inj. HAI s.c - premeal and GRBS
HAI is a short-acting insulin. It works by helping blood sugar (glucose) get into cells so your body can use it for energy. GRBS stands for General Random Blood Sugar. Due to the deficiency of Vit.B1 patients of wernicke's encephalopathy cannot utilise the glucose in their body and hence require short term insulin to be administered in the presentation to hospital.
Indications:
•chronic alcoholics presenting with diabetic ketoacidosis
•chronic alcoholics presenting in the comatosed state.
Lactulose 30ml/PO/BD
Lactulose is nonabsorbable disaccharide stimulates the passage of ammonia from tissues into the gut lumen and inhibits intestinal ammonia production.
Indications:
•Acute onset of severe encephalopathy symptoms
•Minimal hepatic encephalopathy
•chronic alcoholism
Inj. 2 amp of KCl
KCl is given to treat the hypokalemia present in the patient. Hypokalemic is a common finding in chronic alcoholics.
Indications:
•hypokalemia
•uremia
•metabolic acidosis
•insulin therapy given
•intermittent iv infusions
3)Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
4) What is the reason for giving thiamine in this patient?
Answer:
Chronic alcoholics have high incidence of vitamin B1(thiamine) deficiency and this is the main reason for the wernicke's encephalopathy in this patient cjasing a lot of neurological symptoms in the patient. Thiamine is thus given as a prophylactic and treatment therapy of wernicke's encephalopathy.
5) What is the probable reason for kidney injury in this patient?
Answer: The main reason for kidney injury in this patient is due to his chronic alcohol consumption.
References :
https://www.kidney.org/atoz/content/alcohol
6) What is the probable cause for the normocytic anemia?
Answer:
The patient has chronic alcoholism which lead to a chronic kidney disease which might have been the cause for normocytic anemia.
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why
Answer:
Chronic alcoholism is a main cause of peripheral neuropathy which may be a main cause for the development of repeated ulcers on the foot.
B)
Patient details:
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
a) Symptomatology in the patient in terms of an event timeline:
Tab Veratin 8 mg PO TID
Mechanism of action : The active ingredient of Betahistine is Betahistine hydrochloride or Betahistinedemesytate. Betahistine is one of the few drugs known which is said to improve the microcirculation of the inner ear. It works as a histamine analogue through 2 modes of action(1) agonist of H1 receptors and (2) antagonist of H3 receptors. It has a weak effect on H1 receptors but strong effect on H3 receptors.Betahistine is thought to work by increasing the blood flow around the inner ear. This reduces the amount of fluid in the inner ear and prevents symptoms from developing.
Indications :
•Ménière's syndrome
•vertigo
•tinnitus
•hearing loss and
•nausea
b) Anatomical localisation :
Cerebellar infarct revealed on the CT Scan images.
c) Primary etiology in causing the disease :
Patient being a chronic hypertensive and a chronic alcoholic might have been the primary etiology in causation of the disease.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer :
Inj. Zofer 4mg IV/TID
Mechanism of action:
Zofer Tablet works by inhibiting the action of a chemical substance named serotonin, which is responsible for inducing nausea and vomiting. Ondansetron binds to a receptor known as 5-HT₃, thus inhibits the binding of serotonin to it and prevents vomiting and nausea
Indications :
•Nausea and vomiting due to certain medical conditions like stomach upset
•Nausea and vomiting caused due to any surgery, cancer drug therapy or radiotherapy.
Tab. Ecosprin 75mg PO/OD
Mechanism of action :
Ecosprin provides the antiplatelet action by irreversibly inhibiting the formation of thromboxane A2, via acetylation of platelet cyclooxygenase.
Indications:
•For prevention of blood clot formation in individuals with a high risk of clotting in blood vessels.
•For prevention of heart attack.
Tab. Atorvastatin 40mg PO/HS
Mechanism of action:
Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver
Indications : Clinicians may choose to offer a low- to moderate-dose statin to certain adults without a history of CVD when all of the following criteria are met: 1) they are aged 40 to 75 years; 2) they have 1 or more CVD risk factors (i.e., dyslipidemia, diabetes, hypertension, or smoking); and 3) they have a calculated 10-year risk of a cardiovascular event of 7.5% to 10%
Compared with placebo, standard-dose statin treatment resulted in a significant relative risk (RR) reduction of 15% in the occurrence of any major cardiovascular or cerebrovascular event
Tab. Clopidogrel 75mg PO/OD
Mechanism of action: The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation.
Indications : FDA-approved indications for clopidogrel include:
Use during a percutaneous coronary intervention (PCI) for acute coronary syndrome (ACS) and stable ischemic heart disease.
The CREDO trial, PCI-CURE subset analysis, and ISAR studies support the benefit of early treatment with clopidogrel before PCI.
Inj. Thiamine 1 amp in 100ml NS PO/BD
Mechanism of action : Thiamine is useful in chronic alcoholics in preventing Wernicke encephalopathy in , an acute disorder due to thiamine deficiency manifested by confusion, ataxia, and ophthalmoplegia, as well as the chronic Korsakoff syndrome, which is manifested by memory impairment and amnesia.
Indications :
• In conditions of thiamine deficiency commonly noticed in chronic alcoholics with presenting symptoms of beri beri and wernicke's encephalopathy
• In malabsorption disorder caused due to chronic alcoholism.
Thiamine is commonly used for the treatment of wernicke's encephalopathy .
3) Did the patients history of denovo HTN contribute to his current condition?
Answer :
Yes , the incidence of strokes increased in the presence of hypertension. Hence the hypertension in the patient might have contributed to the present condition
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
Answer :
Heavy drinking should be considered as one of the risk factors for hemorrhagic stroke. In contrast to the protective effect of mild-to-moderate alcohol use against ischemic strokes, moderate drinking might result in an increased risk of hemorrhagic strokes.
C)
Patient details :
QUESTIONS :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer :
8 months back:
-Apparently normal
-Then she developed bilateral pedal edema which are gradually progressing and was present on both sitting and standing positions
-Relieved on taking medication
6 days back:
-Pain radiating along left upper limb which was dragging in nature
-Aggravated during palpitations and relieved on taking medication for palpitations
-Chest pain associated with chest heaviness
5 days back:
-Palpitations which were sudden in onset, more during night time
-Aggravated on lifting weights, speak continuously
-Relieved by drinking more water and taking medication
-Dyspnoea during palpitations (NYHA-CLASS-3)
-No history of fever/vomiting/diarrhoea/muscle pain
b) Anatomical localisation :
c) Primary etiology in the problem :
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
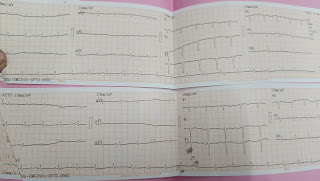
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
Answer :
a)Ecg findings :
•3-3.5 meq/L : Flatenning of T wave , Prominent U wave and Prominent QT interval
•2.5-3 meq/L : Sagging or depression of ST segment
• <2.5 meq/L : QRS widening , increased risk of arrythmia , PR prolongation.
b) Symptoms of hypokalemia :
•Weakness
•Fatigue
•Muscle cramps or twitching
•Constipation
•Arrhythmia
•Worsening diabetes control or polyuria.
•Palpitations.
•Psychological symptoms (eg, psychosis, delirium, hallucinations, depression)
D)
Patient details:
QUESTIONS:
1) Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Answer :
Relationship Between Seizure and Stroke.
Seizures are actually more common after stroke. Statistics show that seizures afflict 22 percent of people who suffer from strokes. They are important to watch out for as they indicate malfunctions in brain activity and cause an altered state of awareness for a stretch of time.
2) In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
E)
Patient details:
QUESTIONS :
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
Answer :
Alcohol induced cerebellar degeneration is the commonest type of acquired toxic ataxia. The onset of the cerebellar symptoms usually occurs at middle age, with a significant history of chronic alcohol abuse.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
Answer :
The most probable reason for the Intracranial bleed in the patient might be chronic alcoholism. Chronic alcoholism has been equated to increased risk and chances of causing intracranial bleeding.
F)
Patient details:
QUESTIONS :
1) Does the patient's history of road traffic accident have any role in his present condition?
Answer :
The findings are indicative of Acute infarct in the Middle Cerebral Artery territory without any evidence of hemorrhages.
These infarcts might be consistent with the finding in the history of the patient which has a road traffic accident
2)What are warning signs of CVA
Answer:
The five warning signs of CVA/Stroke are:
•Sudden onset of weakness or numbness on one side of the body
•Sudden speech difficulty or confusion
•Sudden difficulty seeing in one or both eyes
•Sudden onset of dizziness, trouble walking or loss of balance
•Sudden, severe headache with no known cause
3)What is the drug rationale in CVA?
Answer:
The Role of Medications in General Supportive Care:
•Antihypertensives
In the setting of AIS, many patients will have elevated blood pressure for the first 24–48 hours.
•Insulin
Hypoglycemia can cause focal neurologic signs that mimic stroke and can itself lead to brain injury. .
Rationale of drugs in the treatment of Acute Ischemic Stroke:
•Thrombolysis
Intravenous administration of alteplase is the only US Food and Drug Administration (FDA)-approved medical therapy for treatment of patients with acute ischemic stroke. .
•Anticoagulants
Data suggest that urgent anticoagulation in unselected acute ischemic stroke patients leads to symptomatic intracranial hemorrhage that outweighs any potential benifit
•Antiplatelet Agents
Aspirin irreversibly inhibits cyclooxygenase, which prevents the conversion of arachidonic acid to thromboxane A2 (TXA2)..
4)Does alcohol has any role in his attack?
Answer :
In the patient history it has been described that the patient is an occasional alcohol consumer and also he had not consumed any alcohol prior to the attack indicates that alcohol might not have any role to play in the causation of this disease.
5)Does his lipid profile has any role for his attack??
Answer :
Studies have demonstrated a trend toward a higher risk of stroke with lower HDL-C and support HDL-C as an important modifiable stroke risk factor. In patients with recent stroke or transient ischemic attack and no coronary heart disease, only lower baseline HDL-C predicted the risk of recurrent stroke
G-Details to patient link:
1)What is myelopathy hand?
answer:
There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
2)What is finger escape?
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi. ... This finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign".
3)What is Hoffman's sign?
A positive Hoffmann's sign is suggestive of corticospinal tract dysfunction localized to the cervical segments of the spinal cord.[3] In this regard, it is analogous to the Babinski sign.
Conditions such as multiple sclerosis, hyperthyroidism, and anxiety will also result in a positive sign.
H) Link to patients details:
Possible questions:
1) What can be the cause of her condition ?
Ans; Presence of cortical vein thrombosis with hemorrhagic venous infarction in right posterior temporal lobe and also Iron deficiency anaemia
2) What are the risk factors for cortical vein thrombosis?
Ans; For children and infants Problems with the way their blood forms clots
Sickle cell anemia
Chronic hemolytic anemia
Beta-thalassemia major
Heart disease — either congenital (you're born with it) or acquired (you develop it)
Iron deficiency
Certain infections
Dehydration
Head injury
For newborns, a mother who had certain infections or a history of infertility
For adults
Pregnancy and the first few weeks after delivery
Problems with blood clotting; for example, antiphospholipid syndrome, protein C and S deficiency, antithrombin III deficiency, lupus anticoagulant, or factor V Leiden mutation
Cancer
Collagen vascular diseases like lupus, Wegener’s granulomatosis, and Behcet syndrome
Obesity
Low blood pressure in the brain (intracranial hypotension)
Inflammatory bowel disease like Crohn’s disease or ulcerative colitis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Ans Missed medication
Lack of sleep
Stress
Menstruation About half of women of childbearing age with epilepsy have increased seizures around their period. This is most likely due to hormonal changes that occur during your monthly cycle.
Herbal medications — as well as the herbs that go into many dietary supplements — can actually cause seizures or worsen side effects of seizure medication. The same goes with essential oils. Certain ones, such as juniper and umbrella plant, have been known to induce seizures.
Vitamin B6 (pyridoxine) deficiency is the only type of vitamin deficiency that’s been proven to potentially cause or worsen seizures
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Ans ; Inj sodium valproate and Inj phenytoin have anti platlet activity
3) CARDIOLOGY:
A) A 78 yr old male patient, came to the OPD with chief complaints of shortness of breath, chest pain, pedal edema and facial puffiness.
Patient details:
Questions:
1. What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
ANSWER:
Heart failure with preserved ejection fraction (HFpEF) occurs when the lower left chamber (left ventricle) is not able to fill properly with blood during the diastolic (filling) phase. The amount of blood pumped out to the body is less than normal. It is also called diastolic heart failure.
Heart failure with reduced ejection fraction happens when the muscle of the left ventricle is not pumping as well as normal. The ejection fraction is 40% or less. The amount of blood being pumped out of the heart is less than the body needs.
HEART FAILURE WITH PRESERVED EJECTION FRACTION
HEART FAILURE WITH REDUCED EJECTION FRACTION
Risk factors
Elderly
Females> males
Hypertension
Diabetes mellitus
Obesity
Male>female
Dyslipidemia
Smoking
Myocardial necrosis/ inflammation
Organ level
Concentric LV remodeling
High LV mass/volume
Eccentric LV remodeling
Low LV mass/volume
Molecular level
Cardiomyocyte hypertrophy
Collagenolysis
Interstitial fibrosis
Titin isoform shift to N2B( stiff spring)
Cardiomyocyte loss
Replacement fibrosis
Titin isoform shift to N2BA (compliant spring)
2. Why haven't we done pericardiocentesis in this patient?
ANSWER: It is avoided in the patient because:
There is no cardiac tamponade in the patient.
The pericardial effusion is present as a small pocket .
The effusion was noted to be resolving on its own.[ resolved from 2.4cm to 1.9cm]
Indications for pericardiocentesis:
Cardiac tamponade is a class I indication for PC according to the European Society of Cardiology guidelines for management of pericardial diseases.
A large (>20 mm) pericardial effusion may also be considered for PC (Class IIa recommendation)
PC is not typically performed when an effusion is noted to be resolving on its own or less invasive methods can be used to make the diagnosis and treat the source of the effusion.
3. What are the risk factors for development of heart failure in the patient?
ANSWER: Risk factors are:
Diabetes mellitus
Old age
Diastolic filling impairment
Valvular heart disease
Collapsing left ventricle
Chronic alcoholic
Smoking
4. What could be the cause for hypotension in this patient?
ANSWER: It may have been due to thickening of his visceral pericardium secondary to TB , restricting his heart to expand leading to hypotension.
B) A 73 yr male patient presented to OPD with chief complaints of pedal edema, shortness of breath and decreased urine output.
Patient details :
1. What are the possible causes for heart failure in this patient?
ANSWER: The possible causes for HFpEF are:
Hypertension
Diabetes mellitus
Chronic kidney disease
Obesity
Anemia of chronic disease
2. What is the reason for anemia in this case?
ANSWER: Anemia may have been caused due to:
Inadequate erythropoietin due renal failure ( CKD)
Nutritional deficiency of iron
Decreased RBC production ( Chronic alcoholic since 40years)
Overall the anemia may be due to chronic disease or chronic alcoholism.
3. What is the reason for blebs and non healing ulcer in the legs of this patient?
ANSWER: The blebs may be caused as a complication of diabetes mellitus.
Non healing ulcer is caused due to delayed wounding healing because of:
Diabetes mellitus ( narrowing of blood vessels leading to decreased perfusion)
Heart failure (due to lower perfusion and oxygenation in the extremities)
Anemia ( halt or slow the wound healing stages, which leaves patients more susceptible to other complications such as wound infection.)
4. What sequence of stages of diabetes has been noted in this patient?
ANSWER: stages of diabetes type 2 noted in the patient are:
Stage 1: insulin resistance
Stage 2: prediabetes
Stage 3: diabetes type 2
Stage 4: microvascular complications ( retinopathy, nephropathy, neuropathy)
C) A 52yr old male came to the OPD with the chief complaints of decreased urine output and shortness of breath at rest and facial puffiness.
Patient details:
1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER:
Timeline:
Facial puffiness - since 2-3 years
🡳
Shortness of breath- 1year ago
( grade 2 , diagnosed to be hypertensive)
🡳
Shortness of breath- since 2days
( started as grade 2 and progressed to grade 4)
🡳
Decreased urine output- since 2days
🡳
Anuria- since morning
The patient has a history of surgery for inguinal hernia 10 years ago and pain at surgical site which aggravated since 3years.
The anatomical location of the thrombi are:
Left atrial appendages
Left atrium
There is presence of dilation of all heart chambers and IVC.
Etiology: The causes of atrial fibrillation with thrombus formation in the patient are:
Pulmonary artery hypertension
Congestive cardiac failure
2. What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Dobutamine Inj:
Dobutamine increases contractility, which leads to decreased end-systolic volume and, therefore, increased stroke volume compared to placebo. The larger stroke volume leads to an increase in cardiac output of the heart.
Mechanism of action:
dobutamine is used because of its inotropic effects on the myocardium through binding and activating the beta-1 receptors.
Indications:
It is indicated in:
Temporary intravenous inotropic support until resolution of the acute inducing factors or the patient receives more definitive treatment.
Continuous intravenous form for inotropic support to bridge patients with late-stage heart failure, stage D.
Short-term for those hospitalized patients with severe systolic dysfunction who present with low blood pressure .
Decompensated congestive heart failure because of the sympathomimetic effects.
Digoxin:
Patients with systolic congestive heart failure with normal sinus rhythm, digoxin appears to have a neutral effect on mortality especially if close digoxin level monitoring is employed compared to placebo.
Mechanism of action:
Digoxin’s primary mechanism of action is through inhibition of sodium-potassium adenosine triphosphatase (ATPase). Its role in heart failure patients is based on its inotropic properties, due to inhibition of sodium-potassium ATPase which leads to increased intracellular calcium concentrations through the sodium-calcium exchanger.
digoxin has a parasympathetic effect on the sinoatrial node, by decreasing the automaticity as well as on the atrioventricular conduction system by decreasing conduction and increasing the effective refractory periods.
Indications:
ACC/AHA and ESC guidelines recommendation on the use of digoxin in heart failure with reduced ejection fraction and normal sinus rhythm.
Digoxin can be considered in combination with a beta blocker and/or nondihydropyridine calcium channel blocker when the ventricular rate is poorly controlled in patients with underlying left ventricular dysfunction.
Use of digoxin in the acute management of patients who present with acute ST elevation myocardial infarction.
Heparin 5000:
The role of heparin for prevention of ischemic stroke and systemic embolism in high-risk patients with nonvalvular AF is better compared to placebo.
Mechanism of action:
Heparin is a sulfated polysaccharide with a molecular weight range of 3000 to 30 000 Da (mean, 15 000 Da). It produces its major anticoagulant effect by inactivating thrombin and activated factor X (factor Xa) through an antithrombin (AT)-dependent mechanism. By inactivating thrombin, heparin not only prevents fibrin formation but also inhibits thrombin-induced activation of platelets and of factors V and VIII.
Indications:
Heparin is used to prevent acute thrombosis after coronary thrombolysis.
Heparin represents an effective alternative to warfarin for antithrombotic prophylaxis.
Carvediol:
Beta-blockers have been shown to improve survival in patients with chronic heart failure compared to placebo.
Mechanism of action:
Carvedilol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart.
Indication:
Left ventricular dysfunction
Hypertension
Treatment of mild-to-severe heart failure of ischemic or cardiomyopathic origin
Acitrom:
It has been documented that prolonged oral anticoagulation with proper control of INR significantly reduces the risk of cerebral stroke compared to placebo in patients with atrial fibrillation.
Mechanism of action:
It exerts anticoagulant action by preventing the regeneration of reduced Vit K by interfering with Vit k epoxide reductase.
Dytor:
Toresamide is superior to placebo for cardioversion of AF, and even though the onset of conversion is delayed, its efficacy is similar at 24 h compared with class Ic drugs.
Mechanism of action:
Toresamide causes excretion of sodium chloride and water by inhibiting sodium and chloride reabsorption in the ascending loop of Henle and distal collecting tubule. The effect is caused by blocking the chloride-binding site of the Na+/K+/2Cl- cotransport mechanism.
Indications:
edema / fluid overload
hypertension
3. What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
ANSWER:
Pathogenesis:
The inability of the failing heart to generate forward flow, thus resulting in prerenal hypo perfusion. Inadequate renal afferent flow activates the RAAS axis, the sympathetic nervous system, and arginine vasopressin secretion, leading to fluid retention, increased preload, and worsening pump failure.
This patient has type 4 cardiorenal syndrome.
4. What are the risk factors for atherosclerosis in this patient?
ANSWER:
Risk factors for this patient are:
Diabetes type 2
Hypertension
Age- 52years
5. Why was the patient asked to get those APTT, INR tests for review?
ANSWER:
The aPTT used to be the most commonly used method to monitor the effect of UFH therapy. UFH potentiates the activity of antithrombin and covalently neutralizes thrombin and activated factor X (anti-FXa).
We regularly monitor the INR of people using anticoagulants in order to balance the risk of excessive bleeding (when the INR is too high, meaning that the blood is too thin) against the risk of clotting or thrombosis (when the INR is too low or the blood is too thick).
D)A 67 year old female patient came to the OPD with C/O shortness of breath (SOB) since 1/2hour.
Patient details:
1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER:
Heart burn like episodes- since 1year
🡳
Diagnosed with TB- 7 months ago
🡳
shortness of breath- 30 minutes ago
Etiology:
Diabetes mellitus type 2
Hypertension
High cholesterol diet
2. What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANSWER:
MET- XL:
Beta-blockers have been shown to improve survival in patients with chronic heart failure compared to placebo.
Mechanism of action:
Metoprolol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart.
Indications:
Left ventricular dysfunction
Hypertension
Treatment of mild-to-severe heart failure of ischemic or cardiomyopathic origin
NSTEMI
3. What are the indications and contraindications for PCI?
ANSWER:
Clinical indications for PCI include the following:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
High risk stress test findings.
4. What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on over testing and overtreatment important to current healthcare systems?
ANSWER:
The 2013 American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines for the management of STEMI consider primary PCI as a class I indication in STEMI patients within 12 hours’ of initial symptom onset.2 Beyond this timeframe PCI does not show benefit, as shown in the occluded artery trial which evaluated PCI benefit among stable, high-risk patients with persistent total coronary occlusion after MI. The study concluded that PCI performed from 3 to 28 days after MI does not decrease the incidence of death, reinfarction or New York Heart Association (NYHA) class IV heart failure but it is associated with higher rates of both procedure-related and true ST elevation reinfarction.3 A retrospective analysis of the clinical data revealed The Thrombolysis in Myocardial Infarction (TIMI) Risk Score of 4 predicting a 30-day mortality of 7.3% in this patient. Late PCI leads to the increased risks of periprocedural complications, long-term bleeding, and stent thrombosis.
E) A 60year old Male patient, came to the OPD with the chief complaint of chest pain , giddiness and profuse sweating .
Patient details:
1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER:
Chest pain- since 3days
🡳
Giddiness - since morning
🡳
Profuse sweating- since morning
Anatomical location of the lesion is inferior wall of the heart.
Etiology:
Smoking
Diabetes mellitus
Hypertension
2. What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANSWER:
Aspirin:
A lower incidence of nonfatal myocardial infarction in the aspirin group compared with the placebo group.
Mechanism of action:
Acetylsalicylic acid (ASA) blocks prostaglandin synthesis. It is non-selective for COX-1 and COX-2 enzymes . Inhibition of COX-1 results in the inhibition of platelet aggregation for about 7-10 days (average platelet lifespan). The acetyl group of acetylsalicylic acid binds with a serine residue of the cyclooxygenase-1 (COX-1) enzyme, leading to irreversible inhibition. This prevents the production of pain-causing prostaglandins. This process also stops the conversion of arachidonic acid to thromboxane A2 (TXA2), which is a potent inducer of platelet aggregation.
Indications:
Reducing the risk of cardiovascular death in suspected cases of myocardial infarction
Reducing the risk of a first non-fatal myocardial infarction in patients, and for reducing morbidity and mortality in cases of unstable angina and in those who have had a prior myocardial infarction
Reducing the risk of transient ischemic attack
Atorvas:
High-intensity statin therapy might be beneficial in patients with MI compared to placebo.
Mechanism of action:
Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver.
Indications:
Reduce the risk of non-fatal myocardial infarction.
Reduce the risk of fatal and non-fatal stroke.
Reduce the risk for revascularization procedures.
Reduce the risk of hospitalization for CHF.
Reduce the risk of angina.
Clopibb:
Among patients with ST elevation MI, treatment with clopidogrel was associated with a reduction in mortality and in the composite of death, MI, or stroke compared with placebo.
Mechanism of action:
The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible.
Indications:
Use during a percutaneous coronary intervention (PCI) for acute coronary syndrome (ACS) and stable ischemic heart disease.[4][5][6]
Primary prevention of thromboembolism atrial fibrillation
STEMI
PTCA:
Clinical indications for PCI include the following:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
High risk stress test findings
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
ANSWER: The secondary PTCA was unnecessary in the patient as he already crossed the window period of 12 hours and was doing fine without the PTCA.
F) An 87 year old male patient presented to the OPD with chief complaints of shortness of breath, constipation and decreased urine output.
Patient details:
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
ANSWER: The reason for shortness of breath in the patient may have been hypovolemia which was treated with IV fluids.
2. What is the rationale of using toresamide in this patient?
ANSWER: Loop diuretics such as toresamide improve some hemodynamic parameters and dyspnea due to congestion, i.e., water and salt retention. This may have been the reason behind the use of toresamide in this patient.
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
ANSWER: ceftriaxone was given as we suspected pyogenic infection because of the presence of pus cells in the urine. It was given as treatment for UTI and not prophylactic.
4-GASTROENTEROLOGY
A- Patient details link:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
TIMELINE OF EVENTS-
. 5YEARS AGO : An episode of pain abdomen and vomitings,
Treated conservatively at a local hospital.
Stopped alcohol consumption.
. Symptom free for almost 3 YEARS
. Patient started consuming alcohol, this lead to recurrent episodes of pain abdomen and vomiting.
.1 YEAR AGO : 5-6 episodes of pain abdomen and vomitings
Treated by a RMP.
.1 WEEK AGO : Binge of alcohol,
. SINCE 1 WEEK: following this he had pain abdomen and vomiting
. SINCE 4 DAYS : High grade fever with chills and rigors
Developed constipation
Burning MICTURITION associated with subrapubic pain , increased frequency and urgency.
Anatomical localisation- GASTROINTESTINAL SYSTEM.( stomach and pancreas mainly as the symptoms suggest)
Etiology: the patient is a chronic alcoholic, episodes of abdominal pain and vomiting are following alcohol consumption .
THEREFORE it is heavy drinking that has led to the above condition in the patient.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Drugs used in this patient -
1) ING. MEROPENEM ; TID for 7 days
. Meropenem is a broad spectrum carbipenem antibiotic used to treat abdominal and skin infections.
2) ING. METROGYL 500 mg IV TID for 5 days
Composition- METRONIDAZOLE.
.Metronidazole belongs to Nitroimidazole group of antibiotics, is used to treat gastrointestinal infections, skin and blood infections.
Optimal Treatment for Compliated Intra-abdominal Infections ..
Based on the above study metronidazole when combined with another antimicrobial agent is more effective in the treatment of complicated intra abdominal infections ( particularly those caused by ENTEROBACTERIACEAE MEMBERS as they are resistant to carbipenem).
3) ING. AMIKACIN 500 mg IV BD for 5days
.AMIKACIN is an amino glycoside antibiotic used in the treatment of serious bacterial infections.
All the above three antibiotics are given to control infection and prevent sepsis in the patient.
4) ING. OCTREOTIDE 100 mg SC , BD
Octreotide is a long acting analogue of Somatostatin
.It inhibits exocrine secretion of the pancreas, also has anti inflammatory and cytoprotective effects.
EFFICACY - Octeotride based on several studies did not provide any symptomatic relief or better cure when compared to other drugs . However it played a significant role in reducing SERUM AMYLASE AND LIPASE LEVELS.
5) ING. PANTOP 40 mg IV , OD
. Pantoprazole a proton pump inhibitor, is known to have pancreatic anti secretory effect.
. Oxidative stress is common in acute pancreatitis- Pantoprazole has a inhibitory effect on hydroxy radicals ( free radicals )- thereby reduces the progression of the disease and helps in reducing oxidative stress.
.PPZ treatment also reduces tissue infiltration of inflammatory cells and acinar cell necrosis in severe AP.
6) ING. TRAMADOL in 100 ml NS IV , OD
Tramadol is an opioid analgesic used to relieve severe pain in acute pancreatitis.
7)ING. THIAMINE 100 mg in 100 ml NS IV , TID*
. Thaimine - Vitamin B1 supplement.
.As the patient is on TPN there is a chance of B1 deficiency
. Wernicke’s encephalopathy ( due to B1 deficiency) has been noted in several cases of pancreatitis so to prevent this Thiamine is given as a prophylactic measure
8) TPN ( Total Parenteral Nutrition )
(TPN) is a method of feeding that bypasses the gastrointestinal tract. Fluids are given intravenously to provide nutrients the body needs. The method is used when a person cannot or should not receive feedings or fluids by mouth.
Parenteral nutrition is used to prevent malnutrition in patients who are unable to obtain adequate nutrients by oral or enteral routes.
9) IV NS / RL at the rate 12l ml per hour
MY APPROACH TO THIS PATIENT AS A TREATING PHYSICIAN:
-When the patients present with the complaints of pain abdomen and vomiting, along with fever, burning micturition, certain investigations must be done.
- First, a general examination must be done, including inspection, percussion, palpation and auscultation of the abdomen.
-Other investigations are CBP (Complete Blood Picture ), LFT( Liver Function tests ), RFT( Renal Function Test ) , Urine analysis, Serum amylase, ABG( Arterial Blood Gas ), Pleural tapping.
-Some imaging studies like, contrast enhanced CT and chest x-ray should be taken as well.
-Now depending on the diagnosis based on the results, chemotherapy must be started. In the case of pancreatitis in this patient, the following treatment can be given.
-- Antibiotic like MEROPENAM, METROGYL, AMIKACIN
-- Fluid levels should be maintained with RL or NS
--Somatostatin analogue like SOMATOSTATIN, decreases the exocrine secretion in the pancreas
-- Proton pump inhibitor
--Vitamins such as Thiamine
--Anti-analgesic such as TRAMADOL
B-Patient details link:
NEHA CASE-
QUESTION: What is causing the patient's dyspnoea? How is it related to pancreatitis?
Pancreatitis is associated with of breath.
Acute pancreatitis is associated with release of inflammatory factors which the lungs, fluid accumulation which is also associated with pancreatitis (the patient was diagnosed pleural effusion) results in shortness of breath.
QUESTION: Name possible reasons why the patient has developed a state of hyperglycaemia.
1. Pancreatitis damages cells that produce insulin and glucagon which are hormones that control the levels of blood sugar. Insufficiency of these hormones can lead to hyperglycaemia
2. Patient is a known alcoholic with increased consumption since 2 months (2 litres of toddy everyday) which could also be a cause of diabetes in the patient. But the patient was never tested before he came to our OPD and did not recall any notable signs.
QUESTION: What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
Excess alcohol consumption is known to elevate LFT’s. alcohol is a known hepatotoxin which effects liver functioning and there is no certain linear relation between the amount consumed and the stage of liver damage.
Sensitivity and specificity of biomarkers in detecting harmful or heavy alcohol consumption
Biomarker AST ALT MCV CDT CDT + GGT CDT + GGT + MCV
Sensitivity 47%-68% 32%-50% 45%-48% 63%-84% 83%-90% 88%
Specificity 80%-95% 87%-92% 52%-94% 92%-98% 95%-98% 95%
AST: Aspartate aminotransferase;
ALT: Alanine aminotransferase;
MCV: Mean corpuscular volume;
CDT: Carbohydrate-deficient transferring;
GGT and CDT are usually taken as specific markers for ALD
QUESTION: What is the line of treatment in this patient?
plan of action and Treatment:
Investigations:
✓ 24 hour urinary protein
✓ Fasting and Post prandial Blood glucose
✓ HbA1c
✓ USG guided pleural tapping
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
C-
Patient details link:
bhavana case- CASE #3
Questions :-
1) What is the most probable diagnosis in this patient?
Differential Diagnosis:
• Ruptured Liver Abscess.
• Organized collection secondary to Hollow viscous Perforation.
• Organized Intraperitoneal Hematoma.
• Free fluid with internal echoes in Bilateral in the Subdiaphragmatic space.
• Grade 3 RPD of right Kidney
The most probably diagnosis is there is abdominal hemorrhage. This will give reasoning to the abdominal distention, and the blood which is aspirated.
2) What was the cause of her death?
After leaving the hospital, the patient went to Hyderabad and underwent an emergency laparotomy surgery. The patient passed away the next day. Cause of her death can be due to complications of laparotomy surgery such as, hemorrhage (bleeding), infection, or damage to internal organs.
3) Does her NSAID abuse have something to do with her condition? How?
NSAID-induced renal dysfunction has a wide spectrum of negative effects, including decreased glomerular perfusion, decreased glomerular filtration rate, and acute renal failure. Chronic NSAIDs use has also been related to hepatotoxicity. While the major adverse effects of NSAIDs such as gastrointestinal mucosa injury are well known, NSAIDs have also been associated with hepatic side effects ranging from asymptomatic elevations in serum aminotransferase levels and hepatitis with jaundice to fulminant liver failure and death.
5) Nephrology (and Urology) 10 Marks
A) Link to patients details:
1. What could be the reason for his SOB ?
Since the patients creatinine levels are very high, functioning of the kidney is reduced. This causes for the accumulation of fluid in the lungs and thus causes SOB
2. Why does he have intermittent episodes of drowsiness ?
In healthy individuals, sleep is accompanied by a decrease in sympathetic activity and an increase in vagal tone that leads to a nocturnal dipping of blood pressure
In any kind of kidney related problem it exhibit sympatho-vagal imbalance due to baroreceptor reflex function impairment in which there is hyperactivity of the sympathetic nervous system and decreased vagal tone
3. Why did he complaint of fleshy mass like passage in his urine?
Creatinine is a normal waste product that the body produces every day during muscle movements and when digesting meat.
When creatinine is very high it probabaly means that high waste product of muscle is being formed and this might result in fleshy mass like passage
4. What are the complications of TURP that he may have had?
Transylurethral resection of prostate (TURP)
Bladder injury
Bleeding
Blood in the urine after surgery
Electrolyte abnormalities
Infection
Loss of erections
Painful or difficult urination
Retrograde ejaculation (when ejaculate goes into the urethra.
B)Patients link details:
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, or excessive activity and impulsivity, which are otherwise not appropriate for a person's age
For a diagnosis, the symptoms have to be present for more than six months, and cause problems in at least two settings (such as school, home, work, or recreational activities).
2. Why doesn't the child have the excessive urge of urination at night time ?
Since the child doesn’t have excessive urge of urination at night but at day there might be a psychiatry related condition
1. Psychosomatic disorder
2. Undiagnosed anxiety disorder
3. How would you want to manage the patient to relieve him of his symptoms?
bacterial kidney infection, the typical course of treatment is antibiotic and painkiller therapy.
If the cause is an overactive bladder, a medication known as an anticholinergic may be used. These prevent abnormal involuntary detrusor muscle contractions from occurring in the wall of the bladder
To treat attention deficit hyperactivity disorder:
For children 6 years of age and older, the recommendations include medication and behavior therapy together — parent training in behavior management for children up to age 12 and other types of behavior therapy and training for adolescents. Schools can be part of the treatment as well.
Methylphenidate A stimulant and a medication used to treat Attention Deficit Hyperactivity Disorder. It can make you feel very ‘up’, awake, excited, alert and energised, but they can also make you feel agitated and aggressive. They may also stop you from feeling hungry.
Amphetamine belongs to a class of drugs known as stimulants. It can help increase your ability to pay attention, stay focused on an activity, and control behavior problems. It may also help you to organize your tasks and improve listening skills.
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology) 10 Marks
A) Link to patients details:
Questions:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
The patient is a known case of Retroviral Disease but she was on her ART since 2 months. There might be a possible chance that her negligence to treat RVD is the cause of her Tracheo esophageal and also TB.
Physical finding
According to CECT there is a fistulous communication between left main bronchi and mid thoracic oesophagus few centimetres below carina
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
Immune reconstitution inflammatory syndrome (IRIS) is a condition seen in some cases of AIDS or immunosuppression, in which the immune system begins to recover, but then responds to a previously acquired opportunistic infection with an overwhelming inflammatory response that paradoxically makes the symptoms of infection worse. The suppression of CD4 T cells by HIV (or by immunosuppressive drugs) causes a decrease in the body's normal response to certain infections. Not only does this make it more difficult to fight the infection, it may mean that a level of infection that would normally produce symptoms is instead undetected (subclinical infection). If the CD4 count rapidly increases (due to effective treatment of HIV, or removal of other causes of immunosuppression), a sudden increase in the inflammatory response produces nonspecific symptomssuch as fever, and in some cases a worsening of damage to the infected tissue
reported to occur in 13%–45% of HIV-infected persons who start ART
7) Infectious disease and Hepatology:
Link to patient details:
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors
present in it ?
What could be the cause in this patient ?
Like any other alcoholic drink, excessive toddy (8.1%)drinking can damage the liver.Even the alcohol content is less than that of wine, the patient has been drinking it since 30 years . Therefore it is the major predisposing factor
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
There can be various mechanisms by which toddy could influence EH virulence. The resident microbial flora in human colon is an important determinant of survival and virulence in EH. Alcohol consumption is known to induce intestinal bacterial dysbiosis, which may in turn alter the activity of EH. Undistilled local alcoholic beverages contain a large number of microorganisms that might have more propensity to cause intestinal dysbiosis. EH lacks mitochondria and obtains its energy from the fermentation of glucose. EH alcohol dehydrogenase 2 (EHADH2) is a key enzyme in this pathway7. Thus, expression of EHADH2 is required for the growth and survival of EH trophozoites in human.
alcohol suppresses the function of Kupffer cells in the liver, which has the important role of clearing the amoeba. This leads to pathogenic invasion leading abscess formation
3. Is liver abscess more common in right lobe ?
Right lobe is more significant part with more blood supply. Therefore liver abscess is more common
4.What are the indications for ultrasound guided aspiration of liver abscess ?
B) Link to patient details:
QUESTIONS:
1) Cause of liver abcess in this patient ?
The patient is occasional toddy drinker which has high amount of Entamoeba histolytica. This causes liver abscess by suppressing the function of Kuffper cells.Therefore Toddy is most probable cause of Liver abscess in this patient
2) How do you approach this patient ?
Hematology:
*Common hematological finding being LEUCOCYTOSIS , indicating inflammation or infection.
* Anemia may be present , or not.
Chemistry:
* Elevated liver enzymes such as AST,ALP are noted .
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
INJECTION. ZOSTUM 1.5 gm IV BD (twice daily)
Zostum is a combination of drugs - SULBACTUM (pencillin) & CEFOPERAZONE(cephalosporin) [Antibiotic]: It is used here to treat if any bacterial cause ( since we can’t take the risk relying on only anti amoebic therapy)
* INJECTION. METROGYL 500mg IV TID ( thrice daily )
Metrogyl has the drug called METRONIDAZOLE[Antibiotic]: For amoebic cause
* INJECTION. OPTINEURIN 1amp in 100 ml NS( Nor
mal Saline) IV OD ( once daily)
Optineurin is a multivitamin drug { A combination of B1,B2, B3, B5,B6, B12 } given here as a supplement
* TAB. ULTRACET 1/2 QID( four times a day)
Ultracet is a combination of drugs - TRAMADOL(opiod analgesic) and ACETAMINOPHEN (analgesic and antipyretic) : Given for pain and fever
* TAB. DOLO 650 mg SOS (if needed) given for fever and pain
* Here ; due to medical therapy his symptoms subsided and clearly we can see it in usg reports ( liquefaction) meaning abcess responded to our medical therapy.
*And the patient was discharged on 10/5/21.
* We donot aspirate the pus since it is self resolving and aspiration is associated with several other complications.
4) Is there a way to confirmthe definitive diagnosis in this patient?
Apart from serological examination which is positive in 94% of the cases..Further confirmation can be done by using Ultrasonography but these are not commonly used
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) 10 Marks
A) Link to patient details:
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Anatomical localisation : Medial canthus of left , Oral cavity and hardpalate, left nasal cavity and left frontal & temporal lobes
Primary etiology
Mucormycetes, the group of fungi that cause mucormycosis, are present throughout the environment, particularly in soil and in association with decaying organic matter, such as leaves, compost piles, and animal dung. 1 They are more common in soil than in air, and in summer and fall than in winter or spring. 2-4 Most people come in contact with microscopic fungal spores every day, so it’s probably impossible to completely avoid coming in contact with mucormycetes. These fungi aren’t harmful to most people. However, for people who have weakened immune systems, breathing in mucormycete spores can cause an infection in the lungs or sinuses which can spread to other parts of the body.
I
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Itraconazole acts by inhibiting the fungal cytochrome P-450 dependent enzyme lanosterol 14-α-demethylase. When this enzyme is inhibited it blocks the conversion of lanosterol to ergosterol, which disrupts fungal cell membrane synthesis. Itraconazole exhibits fungistatic (slows the growth) activity against yeast-like fungi and fungicidal (kills the fungus) activity against Aspergillus spp.
Amphotericin B binds with ergosterol, a component of fungal cell membranes, forming pores that cause rapid leakage of monovalent ions (K+, Na+, H+ and Cl−) and subsequent fungal cell death
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Low oxygen, diabetes, high iron levels, immunosuppression, as well as several other factors including prolonged hospitalisation with mechanical ventilators, creates an ideal milieu for contracting mucormycosis,
Contamination in pipes of the oxygen cylinders
unhygienic masks" and poorly ventilated rooms could be a contributing factor
history of exhibiting poor hygienic practices, including wearing unwashed masks for a long time.
irrational use of steroids
Mucormycosis is more common among people whose immunity has lowered due to COVID, diabetes, kidney disease, liver or cardiac disorders, age-related issues, or those on medication for auto-immune diseases like rheumatoid arthritis.
9)INFECTIOUS DISEASES(COVID-19)
10) I thank Dr.Rakesh Biswas sir ,as this project was very informative and this evidence based learning helped me to change my approach towards medicine subject.I think this is the best way of gaining knowledge rather than studying books.Thank you sir.

Comments
Post a Comment