This is an online E log book to discuss our patient's de-identified health data shared after taking her guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E-log also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.B Madhu kumar
ROLL No : 18
INTERN
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, Clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE:
69 year old male came to the casualty with the
CHIEF COMPLAINTS
1. Decreased Urine output since yesterday.
2. Shortness of Breath.
HOPI:
The patient was a daily wage labourer who stopped working 10 years ago, had complaints of pedal edema since 20 days , decreased Urine output since 3 days , Anuria since 1 day and shortness of breath since 1 day.
The patient was apparently asymptomatic 20 days ago, developed pedal edema which gradually progressed upto knee, pitting type. Went to local hospital and used some tablets after which he had polyuria but the pedal edema did not subside. Since today morning he developed Shortness of breath ( grade 4) and Anuria
No complaints of chest pain , palpitations ,orthopnea ,PND ,fever, vomiting,loose stools.
No complaints of giddiness
Complaints of cough with sputum.
PAST HISTORY:
K/C/O DM since 5 years for which he was on Tab. Metformin.
H/O Leg Trauma 1 year ago , fracture was operated and it lead to Non union.
Bed ridden since 1 year , sits on his own but not able to work.
H/O seasonal SOB since many years associated with wheeze, cough on and off.
PERSONAL HISTORY:
DIET: Mixed
SLEEP: Adequate
BOWEL AND BLADDER: Regular
ADDICTIONS :
Alcoholic since 40 years ( 90 ml daily)
Beedi smoking - 2-3/ day daily since 40 years.
ALLERGIES : No
FAMILY HISTORY:
Insignificant
GENERAL EXAMINATION:
Patient is concious, coherent and co-operative and oriented to time and place.
PALLOR : Absent
ICTERUS:Absent
CYANOSIS:Absent
CLUBBING:Absent
LYMPHADENOPATHY:Absent
EDEMA: B/L Pedal Edema ( pitting type ) upto knees .
VITALS:
Temperature: 98.9° F
Pulse Rate : 96 Bpm
RR: 21 CPM
BP : 140/90 mm Hg
Spo2 : 70 % on Room Air ,98% on 13 litres of O2 .
GRBS : 60 mg /dl.
SYSTEMIC EXAMINATION:
CVS:
No Thrills
S1 and S2 - Heard
No cardiac murmurs
RESPIRATORY SYSTEM:
BARREL SHAPED CHEST
BAE - PRESENT
B/L CREPTS - PRESENT
WHEEZE - present ( B/L infraclavicular, inframammary, intra axillary areas.)
ABDOMEN:
Shape of Abdomen- Normal
Tenderness - present in umbilical area.
No palpable mass .
Normal hernial orifices.
Not palpable spleen and liver .
CNS:
Level of consciousness: Normal
Speech : Normal
No signs of meningial irritation
Glasgow coma score: 15/15
INVESTIGATIONS:(DAY 1)
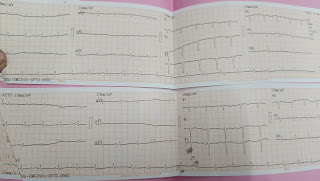
ECG:




































Comments
Post a Comment