Acute pancreatitis
- Get link
- X
- Other Apps
ACUTE PANCREATITIS
A 32 YEAR OLD MALE WITH PAIN ABDOMEN
B.Madhu Kumar
Roll no :11
9th semester
9th semester
30th October 2021
This is an online E-Log book to discuss our patient's de-identified data shared after taking his/her/Guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve these patient's clinical problems with collective current best evidence-based inputs. This E-log also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, Clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE:
A 32 Year old male, resident of XXX , Lorry driver by occupation Presented to the OPD on 29/10/2021 with Pain Abdomen.
CHIEF COMPLAINTS:
1. Pain abdomen since one day
2. Vomiting since one day (2 episodes)
3. Constipation since one day
HOPI:
The patient was apparently asymptomatic 4 years ago and then developed-
PAIN ABDOMEN- He went to a local hospital and was diagnosed with acute pancreatitis and treated. He was asked to stop consuming alcohol. He continued to have alcohol occasionally.
SEPTEMBER 2021
He had similar complaints and was treated.
OCTOBER 2021
29/10/2021- He presented to the OPD with-
- PAIN ABDOMEN- in Epigastrium and left hypochondrium since 1 day
Aggravated on drinking and no relieving factors.
There is no positional and diurnal variation.
- VOMITING - The patient had associated nausea and vomiting.
2 episodes, non- projectile, non- bilious, contents are food particles.
- CONSTIPATION- since one day
- SOB- Grade 4
- No h/o Fever.
PAST HISTORY:
The patient had similar complaints 4 years back, took prescribed medications and was asked to stop consuming alcohol.
Not a K/C/O - DM, HTN, Epilepsy, Asthma, TB, CVA.
PERSONAL HISTORY:
- Diet- Mixed
- Appetite- Loss of appetite is present
- Bowel and bladder movements- Regular
- Sleep- Adequate
- Addictions- H/o alcohol consumption (beer) since 5 years, 2 times a day, stopped 1 month ago.
FAMILY HISTORY
Insignificant
SURGICAL HISTORY:
None
GENERAL EXAMINATION:
INFORMED CONSENT WAS TAKEN and the patient was examined in a well-lit room.
He is conscious, coherent, cooperative, well oriented to time, place and person.
He is well nourished and moderately built.
No Pallor, Icterus, Clubbing, Cyanosis, Koilonychia, Lymphadenopathy, Edema.
VITALS:
- Temperature- Afebrile
- PR- 90 bpm
- RR- 18 cpm
- BP- 100/70 mmHg
SYSTEMIC EXAMINATION:
- CVS: S1, S2 +
- RS: BAE+, NVBS
- P/A: Scaphoid in shape, Soft, Tenderness is present in the epigastric region., Bowel sounds heard, no palpable mass, no free fluid, no bruit.
- CNS: Intact
INVESTIGATIONS:
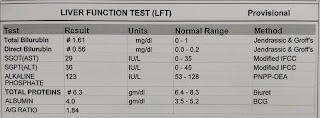
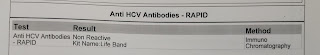
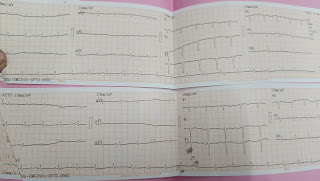
29/10/2021
COMPLETE BLOOD PICTURE
HEMOGRAM
SERUM ELECTROLYTES
LDH
SERUM CALCIUM
COMPLETE URINE EXAMINATION (CUE)
HIV 1/2 RAPID TEST
HBsAg- RAPID
Anti- HCV ANTIBODIES - RAPID
ECG
ULTRASOUND REPORT
COLOUR DOPPLER 2D- ECHO
PROVISIONAL DIAGNOSIS:
Acute Pancreatitis secondary to Alcohol
TREATMENT:
- IVF- NS,RL-150ML/HR
- INJ.PAN.40MG/IV/BD
- INJ. THIAMINE 200MG IN 100ML NS /IV/BD
- INJ.OPTINEURON 1AMP IN 100ML NS/IV/OD
- INJ.TRAMADOL 1AMP IN 100 ML NS/IV / BD
- INJ.ZOFER 4MG /IV/BD
- strict I/O monitoring
- BP,PR, SPO2 Monitoring 4th helt
- GRBS monitoring 6hrly
- inform sos
- Get link
- X
- Other Apps