70 year old male with pleural effusion
MADHU KUMAR B
ROLL no. 11
9th sem
This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians sign informed consent
CONSENT AND DEIDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whomsoever
CASE:
A 70 year old male, who is a daily wage worker came with the
CHIEF COMPLAINTS:
1- Breathlessness (since 20 days)
2-Cough( since 20 days)
3-Fever(since 4 days)
HISTORY OF PRESENTING ILLNESS :
Patient was apparently asymptomatic 20 days back,then he developed
Breathlessness- MMRC - Grade -2 and 3 aggrevated on exertion and on exposure to cold,associated with wheeze no orthopnea and no PND. Relieved on rest.
Cough with expoctoration - mucoid,non foul smelling and non blood stained, increased during night, no postural and diurnal variations relieved on taking medication.
fever,low grade evening rise of temperature,not associated with chills and rigors.
Loss of appetite and loss of Weight are seen.
HISTORY OF PAST ILLNESS:
No H/O similar complaints in the past.
No H/O pulmonary tuberculosis and COVID -19.
No H/O diabetes, hypertension,CAD and epilepsy.
PERSONAL HISTORY:
Appetite: decreased
Diet: mixed
sleep: adequate
Bowel and bladder: Regular
addictions:H/o BD Smoking since 50 years (4-5 BD's per day)
FAMILY HISTORY:
Insignificant.
GENERAL EXAMINATION:
Patient is concious, coherent and oriented to time,place and person.
VITALS:
Pulse rate: 102 BPM
Respiratory rate: 26 CPM
BP: 110/80.
spO2: 96% at room air
SYSTEMIC EXAMINATION:
Respiratory system:
Inspection:
shape of the chest: Bilaterally symmetrical and elliptical.
chest movements: decreased on right side
no kyphosis and scoliosis
no scars( sinuse, visible pulsations and engorged veins)
no usage of accessory muscles.
muscle wasting- present
Palpation:
All inspectory findings are confirmed.
Trachea - shifted to right side.
No local rise of temperature.
chest movements- decreased on right side
spinoscapular distance- same on both sides.
chest expansion-
RT and Lt hemithorax
chest circumference- 31 cm
Transverse diameter- 27cm
anteroposterior diameter-20 cm
Percussion:
Right sided - ICA ( impaired note)
Right sided- SSA ( impaired note)
Auscultation:
Vesicular breath sounds are heard
RT sided - ISA and SSA ( decreased breath sounds)
RT - MA crepitus present.
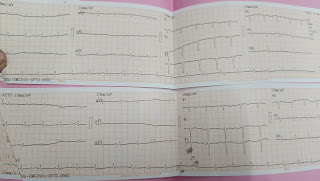
Cardiac Examination:
S1 and S2 - present
Normal heart sounds
No cardiac murmurs.
CNS examination:
Superficial reflexes - present
sensory and motor functions- normal
no focal neurological deficits
Per Abdomen
bowel sounds- heard
soft, non tender,
no organomegaly
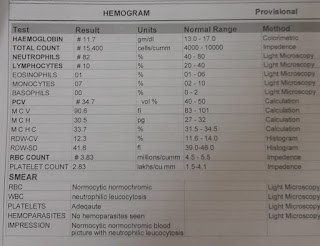
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS:
Right Upper lobe fibrosis with pleural effusion.
TREATMENT:
Inj- AUGMENTIN ( 2g i.v TID)
Inj- PAN -40 mg OD
Inj- Paracetamol- 650 mg BD
ASCORIL - CS ( 2 table spoons)
Nebulization with Budecort ( BD )
Duolen ( TID)
O2 inhalation ( 2-4 lit/ min to maintain SpO2> 94%
Tab - Azithromycin ( 500 mg- OD)









Comments
Post a Comment