52 year old male with fever
This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with n aim to solve those patient clinical problem with collect6current best evidence based input
This Elog also reflects my patient centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan
CONSENT AND DEIDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whomsoever
This is a case of 52 year old male suffering from fever and pedal edema
CHIEF COMPLAINTS:
Complaints of Fever since 2 days
Slurred speech for half an hour 2 days back then he regained his consciousness
B/L Pedal Edema since 2 days
Decreased appetite since 2 days
Abdominal distension
Decreased Urine output since 1 day
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 30 days back then he developed B/L Pedal Edema pitting type for which he used herbal medicine and his edema got resolved.
10 days back he again developed B/L Pedal Edema pitting type associated with abdominal distension and decreased Urine output for which he was treated conservatively
Since 2 days he had complaints of Fever,low grade, intermittent a/w pitting type of pedal edema, abdominal distension and decreased Urine output.
HISTORY OF PAST ILLNESS:
H/O seizures
one episode in childhood
one episode 30 yrs back
one episode 10 yrs back
Not a k/c/o HTM,DM,TB ,ASTHMA, THYROID DISORDERS.
PERSONAL HISTORY:
Appetite: decreased
Diet: mixed
sleep: adequate
Bowel and bladder: Regular
addictions:H/o BD Smoking since 18 years (4-5 BD's per day)
FAMILY HISTORY:
Insignificant.
GENERAL EXAMINATION:
Patient is concious, coherent and oriented to time,place and person.
VITALS:
Pulse rate: 92 BPM
Respiratory rate: 22CPM
BP: 110/90.
spO2: 98% at room air
SYSTEMIC EXAMINATION:
CVS: S1 and S2 - present
CNS: NAD
LUNGS : B/L air entry present
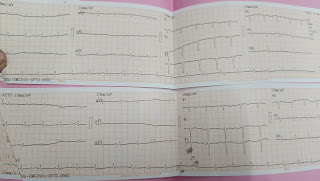
INVESTIGATIONS:
TREATMENT:
1-Inj . Lasix 40mg I.V BD
2-I.V fluids 10 NS 1amp optineuron
I.V Fluids 10 RL @75ml/hr
3- Inj Thiamine 100mg in 100ml NS IV Bd
4- INJ Neomol 2gm I.V
5- Protein powder 2 scoops in 100ml milk TID
6- Tab dolo 650 mg PO SOS.







Comments
Post a Comment